Artificial intelligence technology in healthcare: How it is changing the industry
By Kelly Nguyen | Published: 2025-10-28 10:00:00 | Source: Healthcare Blog
Main takeaways:
- Artificial intelligence (AI) is changing the way healthcare organizations operate, but while most providers believe in its potential, its adoption is uneven.
- As payers use AI to control costs, providers must apply the same technology to address rising claims denials and data quality challenges.
- Experian Health Artificial Intelligence feature and Patient Access Trust Helping providers prevent denials, improve efficiency and enhance financial performance.
Artificial Intelligence is transforming every part of healthcare. In the doctor’s office, it supports faster diagnosis and treatment decisions. At the front desk, assists in verifying coverage and scheduling appointments. In healthcare claims management, AI’s ability to interpret massive amounts of data is changing how claims are reviewed, processed and paid.
But the transition is not without challenges. As providers adopt AI and machine learning (ML) to improve care and operations, payers are using the same technology to control costs and make faster coverage decisions. According to American Medical Association61% of doctors believe that artificial intelligence increases prior authorization denials. The strategic use of AI is the only way to keep pace with progress and maintain competitiveness.
This article explains what providers need to know about using AI in healthcare, including how to use Experian Health Artificial intelligence feature and Patient Access Secretary Using AI to prevent rejections, improve efficiency and enhance financial performance.
Understanding AI and machine learning technology in healthcare
Artificial intelligence refers to technology that performs tasks that require human-like thinking, such as recognizing patterns, interpreting data, and solving problems. It learns from experience, identifies trends that the human eye might miss and makes recommendations based on what users want to achieve.
Machine learning is a subset of artificial intelligence that improves performance over time, helping healthcare organizations turn their complex information into actionable insights. Because these models are trained on each organization’s unique data, they can adapt to local patterns and differences in workflow, making their predictions much more accurate.
Clinical and operational applications
AI and machine learning are now being used in many areas of clinical care, such as:
- Improving diagnosis by analyzing medical images more accurately.
- Accelerate drug discovery by tracking side effects and treatment outcomes.
- Improving surgical safety and precision through robotics.
- Supporting patients in managing their health through wearable devices and remote monitoring.
On the operational side, Artificial intelligence helps employees work smarter and faster. Patient access teams use AI to verify insurance, forecast demand, and manage scheduling, while revenue cycle leaders use it to reduce manual work and improve claims accuracy.
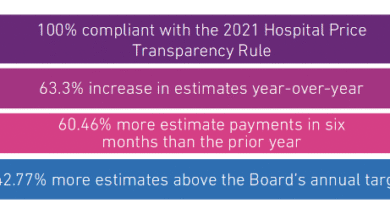
Experian Health Claims Status Report 2025 It found that 69% of organizations using AI solutions experienced fewer rejections or higher resubmission success rates, reflecting measurable gains in both efficiency and financial performance.
How AI technology in healthcare can prevent and reduce claims denials and enhance financial performance
Despite these gains, denials continue to rise, revealing persistent problems with data quality. More than half of providers (54%) in Claims status report They say claims errors are on the rise, and 68% are finding it harder to submit clean claims than they were a year ago.
Furthermore, keeping up with payers’ use of AI is challenging. President of the American Medical Association Bruce A. notes: Scott, “Emerging evidence shows that insurers are using automated decision-making systems to create systematic bulk denials with little or no human review.”
In contrast, on the supplier side, About 90% of cases are denial They require manual rework, which contributes to a widening technology gap that slows down the payment process and puts pressure on already overworked teams. Experian Health’s AI-based solutions can help bridge this gap.
Get accurate data from the start with Patient Access Curator.
Patient Access Secretary It uses artificial intelligence and machine learning to automate front-end eligibility and licensing workflows. It verifies eligibility and insurance coverage and reduces data errors that often lead to final denial. Improving data quality before claim generation helps organizations submit more accurate claims, reduce delays, and deliver a better patient experience.
Predict and prevent rejections with AI Advantage
In a Recent webinarEric Eckhart of the Regional Medical Society (Fresno) and Skyler Early of Schneck Medical Center discuss how Artificial intelligence feature Help them take control of their rejection management strategy and maximize reimbursement.
“What really impressed me about[AI Advantage]is that it’s looking at my data. It’s not looking at Skyler’s data in the Midwest. It’s looking at my data in central California. We have a lot of small payers that do what they want, and they learn from my information, and from my actual denial that’s going on. If the payer switches, the model will follow that and tell me that
– Eric Eckhart, Director of Patient Financial Services at Community Medical Centers
Artificial intelligence feature It takes a two-pronged approach to reduce the risk of rejection and speed up the rework process:
- AI Feature – Predictive Rejection It screens claims before they are submitted and calculates the probability of denial based on historical payment data and real-time undocumented payer behavior. High-risk claims can be amended before submission to reduce the risk of rejection.
- Artificial Intelligence Feature – Rejection Sorting It evaluates and segments rejections based on payment probability and prioritizes the work queue accordingly. It learns from previous decisions to formulate recommendations with increasing precision, so employees can focus on the denials that are most likely to produce results.

Eric Eckhart of the Regional Medical Society (Fresno) and Skyler Early of Schneck Medical Center discuss how AI tools have helped them reduce denials.
Main challenges of applying artificial intelligence technology in healthcare
It is interesting that Claims status survey It indicates that trust in AI outpaces adoption. While 67% of providers believe AI can improve the claims process, only 14% use it to reduce denials. This suggests some caution about the practicalities of applying AI.
For smooth implementation of AI technology, service providers must consider three basics:
- Data quality:AI tools are only as good as the data they analyze. Partnering with a trusted third-party vendor can help providers ensure that data is error-free and usable.
- Merger: New tools should fit easily into existing workflows and systems. A solution provided by a single vendor can mitigate interoperability issues. For example, Artificial intelligence feature Fits seamlessly with Source of claim®and reduce disruption.
- Compliance and security: Solutions must comply with data privacy and security regulations, such as HIPAA, to avoid financial and reputational risks and maintain patient trust.
Frequently asked questions
AI in healthcare uses algorithms and machine learning to analyze data, support clinical decisions, and automate administrative tasks.
AI technology automates claims review processes, predicts denials and prioritizes claims to maximize reimbursement efficiency.
Tools like Experian Health Artificial intelligence feature and Patient Access Secretary Integrate with existing claims management workflows to predict and prevent denials, automate reviews and improve front-end accuracy for faster reimbursement.
As predictive analytics, natural language processing, and automation advance, providers that use AI strategically will see greater efficiency and faster reimbursement. As payers and competitors accelerate adoption of AI, understanding where and how to apply these tools will be essential to remaining adaptable and financially resilient.
What’s next for AI technology in healthcare?
As predictive analytics, natural language processing, and automation advance, providers that use AI strategically will see greater efficiency and faster reimbursement. As payers and competitors accelerate adoption of AI, understanding where and how to apply these tools will be essential to remaining adaptable and financially resilient.
See how Artificial intelligence feature and Patient Access Secretary They help Experian Health customers transform healthcare operations.
(tags for translation) AI Feature
ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ